ADHD Is Often Missed Because Chaos Looks Like Personality
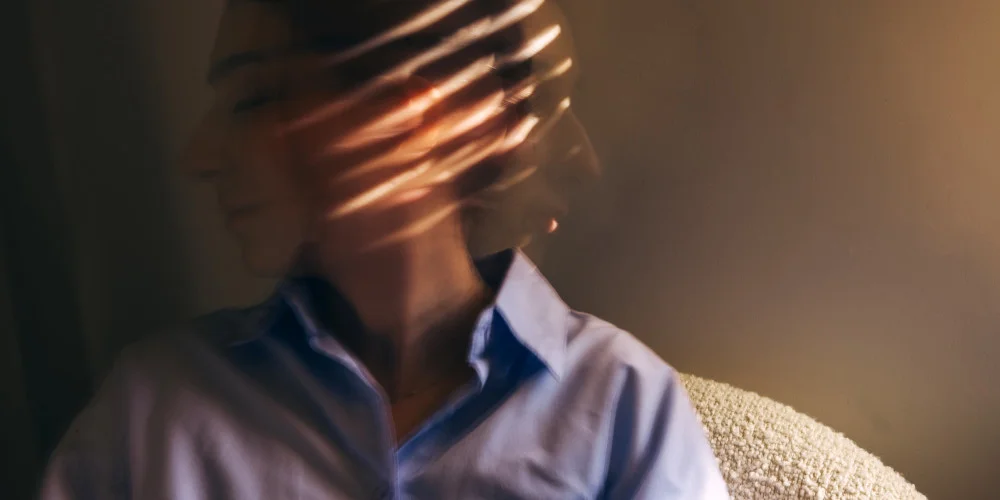
ADHD is one of the most misunderstood conditions in adult mental health, partly because it does not always look like a disorder and often looks like a personality problem instead. People with ADHD are frequently described as intense, unreliable, emotionally reactive, inconsistent, or hard to pin down. These labels stick because the behaviour is visible while the neurological driver behind it is not. In families, schools, and workplaces, the assumption is often that the person could do better if they just tried harder, slowed down, or cared more. Over time this creates a narrative that the problem is attitude rather than brain function.
In South Africa this misinterpretation is amplified by limited access to assessments, cultural expectations around discipline, and systems that reward compliance over adaptability. Many people grow up being corrected constantly without ever being understood. They learn to mask, overcompensate, or swing between overperformance and collapse. By adulthood the chaos feels normal and the idea that something neurological is driving it rarely enters the conversation. ADHD becomes invisible because the person appears functional enough to survive while internally operating in a state of constant friction.
How Stimulation Becomes Survival
The ADHD brain is wired differently when it comes to dopamine regulation, attention, and emotional control. This is not a motivational issue, it is a neurological reality. Tasks that are boring, repetitive, or emotionally flat can feel physically uncomfortable. Thoughts move quickly, emotions spike fast, and the nervous system struggles to settle. Without understanding this, many people instinctively look for external ways to regulate what feels unmanageable inside.
Substances often enter the picture quietly and logically. Alcohol slows racing thoughts and softens emotional intensity. Nicotine sharpens focus and creates brief calm. Cannabis reduces sensory overload and helps with sleep. Stimulants provide clarity and energy. These effects are not accidental and they explain why substance use can feel like relief rather than rebellion. For many people with ADHD, using is not about escape but about functioning. The substance becomes a tool long before it becomes a problem.
The Quiet Pattern of Self Medication
One of the reasons ADHD and addiction are so tightly linked is that the early stages of substance use often appear helpful. Productivity improves, anxiety reduces, sleep becomes easier, and social interaction feels more manageable. Friends and family may even notice positive changes at first, reinforcing the belief that the person has finally found something that works. This delays concern and masks risk.
Over time the cost increases while the benefit decreases. Tolerance builds, consequences emerge, and the original reasons for using are forgotten. By the time addiction is identified, the person is often blamed for poor choices rather than asked why the substance became necessary in the first place. The narrative shifts from coping to failure, leaving the underlying ADHD completely untouched.
Why ADHD Changes the Shape of Addiction
Addiction does not look the same in someone with ADHD as it does in someone without it. Impulsivity increases risk taking and makes early experimentation more likely. Emotional reactivity intensifies cravings during stress, conflict, or boredom. Difficulty with delayed gratification makes long term consequences feel abstract compared to immediate relief. These factors do not excuse harmful behaviour but they do explain why relapse patterns can look different and why standard interventions often miss the mark.
People with ADHD often struggle with rigid routines, long periods of sitting still, and abstract future focused motivation. When recovery is framed as discipline, patience, and compliance, it can feel impossible to maintain. This is not a lack of commitment, it is a mismatch between expectations and neurological capacity.
When Sobriety Feels Worse Than Using
One of the most overlooked realities in addiction treatment is how exposed people with ADHD feel once substances are removed. Detox clears the chemical coping mechanism but does nothing to address the underlying dysregulation. Thoughts race again, sleep becomes disrupted, emotions feel raw, and focus disappears. Without context, this experience can feel like proof that sobriety does not work.
This is where many people quietly relapse. Not because they want chaos but because sobriety without support feels unbearable. When ADHD is untreated, abstinence can feel like punishment rather than progress. People begin to believe they are incapable of living without substances, reinforcing shame and hopelessness.
Why Traditional Rehab Often Misses ADHD Entirely
Many treatment programmes are built around structure, repetition, group participation, and delayed rewards. These approaches work well for some but can unintentionally alienate people with ADHD. Long lectures, passive listening, and rigid schedules can be exhausting rather than supportive. When someone struggles to engage, the assumption is often resistance or lack of willingness.
Without proper screening, ADHD is frequently misdiagnosed as anxiety, depression, or personality issues. The result is treatment that targets symptoms rather than causes. When people leave rehab without tools to manage attention, impulse control, and emotional regulation, relapse is not a mystery, it is predictable.
Medication Fear Misuse and Misinformation
The conversation around ADHD medication in addiction settings is often dominated by fear. There is concern about misuse, dependency, and replacing one substance with another. While these risks exist, avoiding treatment entirely often creates greater harm. Untreated ADHD increases relapse risk, emotional instability, and disengagement from recovery.
Medication is not a cure and it is not appropriate for everyone. However, when properly prescribed and monitored, it can provide stability that makes therapy, routine, and sobriety possible. The decision should be based on individual assessment rather than blanket rules driven by stigma.
What Integrated Treatment Actually Looks Like
Effective treatment for ADHD and addiction does not rely on a single solution. It involves proper assessment, psychoeducation, realistic structure, and skills that match how the brain works. This may include medication, behavioural strategies, coaching, and therapy focused on emotional regulation rather than punishment.
Recovery becomes sustainable when people understand their own nervous system and learn how to work with it instead of against it. This shifts the narrative from failure to adaptation and from willpower to skill development.
The Cost of Treating Addiction Without the Brain Involved
When addiction is treated without acknowledging ADHD, people are left blaming themselves for outcomes that were never fully within their control. They internalise the idea that they are weak, lazy, or broken. This belief does more damage than the substances ever did.
Recognising ADHD does not remove responsibility, it restores context. It allows treatment to address reality rather than expectation. When the brain is finally part of the conversation, recovery stops being a test of character and starts becoming a process of learning how to live without constant internal chaos.